
February 24th marks the second anniversary of the invasion of Ukraine. GRM has been there for 722 of those days.
Responding to an urgent request by the Ukrainian government, GRM is supporting three cohorts of medical teams from the Military Medical Academy, Border GuardsUkraine and National Guards Ukraine, who are tasked with the care of war wounded patients at forward resuscitation facilities and serve as the lead medical trainers for their respective organizations.
During the program, these 15 medical professionals will explore best practice techniques, both in Europe and in the US, for managing complex traumatic injuries, including resource management, team management, and field diagnostics.
The program is tailored to the specific needs and requests of each organization.
Program Objectives
- Explore best practice techniques for war-related injuries at leading international medical facilities
- Implement the new skills and concepts learned, considering the local context
- Help cohorts prepare to share their new kills and knowledge acquired during rotations by implementing TTT (Train-the-Trainer) modules
- Learn the most efficient and up-to-date techniques and approaches in trauma management
- Knowledge-exchange and immersion with foreign colleagues
- Understand how a system of team trauma management works in other environments
Program Schedule
The training cycle as five rotations:
- Rotation #1 took place in Ukraine in January 2024 and focused on Advanced Surgical Skills for Exposure to Trauma (ASSET).
- Rotations #2-4 will be held in US and NATO facilities from March – June 2024.
- Rotation #5 will take place in Ukraine and will focus on applying the new approaches, skills, and knowledge to the local context, ensuring we cover and gap in needs.
Curriculum

While the curriculum will be customized to the physicians’ needs, the following core topics will be covered:
- Resuscitation
- Trauma surgery
- Field surgery
- Mass casualty management
- Amputation
- Burn care
Rotations take place at leading institutions in Chicago, North Carolina, Philadelphia, Amsterdam, Kyiv, Budapest, and beyond.
Program Costs
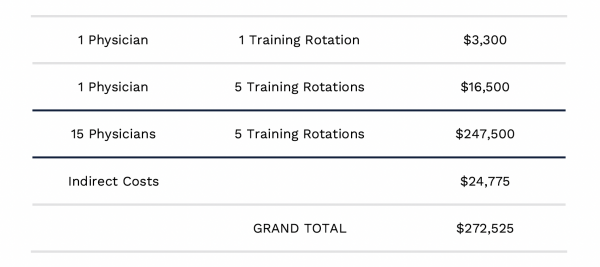
With travel, equipment, and coordination, the cost of the program is $16,500 for each physician for a total of $247,500 for direct costs.
Expected Results
Save lives. Period.
Increased trauma skills for for front line medical professionals immediately means that more lives will be saved and less people will suffer life-altering injuries.
15 medical specialists will be trained on best practice techniques for complex injury management.
New knowledge and immersion at leading international centers working with military trauma.
Save more lives through capacity building.
The graduates will be prepared to work in a TTT format to share their new knowledge with the next cohort of Ukrainian medical professionals.
Increased knowledge in quantity & quality – the graduates will share their knowledge and provide training to future cohorts.
Establish partnerships with international medical institutions fostering multi-lateral relationships.
Contributing to the evolution of front line medical protocols.
“We need to make sure they don’t die, and reach the next point of evacuation.” – Oleksii, Physician
